Tameside Reporter
This week's edition (April 25th.) Click here for previous editions.
-
 One of the teens charged after "traumatising" Ashton bus station robbery has been named
One of the teens charged after "traumatising" Ashton bus station robbery has been named
Police were called to reports of a robbery at Ashton-under-Lyne bus station where two young victims were robbed by a group of five older males.
-
 47 penalty notices issued and one arrest made on Ashton Metrolink in GMP crackdown
47 penalty notices issued and one arrest made on Ashton Metrolink in GMP crackdown
47 Metrolink passengers have received penalty notices for travelling without a valid ticket amid a police crackdown.
-
 Suspended sentence handed to violent Hyde stalker who turned his victim's life "upside down"
Suspended sentence handed to violent Hyde stalker who turned his victim's life "upside down"
A 55-year-old Hyde man has been handed a suspended sentence after stalking a stranger for 14 months.
-
 Ambulance downgraded call out to man who suffered a fit and later died in Tameside Hospital
Ambulance downgraded call out to man who suffered a fit and later died in Tameside Hospital
A man who died in Tameside hospital after suffering a fit may have received emergency help quicker if a different ambulance service had attended to him.
-
 Teenagers arrested on suspicion of robbery in Ashton
Teenagers arrested on suspicion of robbery in Ashton
Police were called to reports of a robbery at Ashton-under-Lyne bus station where two young victims were robbed by a group of five older males.
-
 Secondhand music, books and media shop opens in Mossley
Secondhand music, books and media shop opens in Mossley
Homelessness charity Emmaus Mossley has unveiled a brand-new music, books and media shop within its Secondhand Superstore.
-
 Stalybridge man runs marathon after having a cardiac arrest on the toilet
Stalybridge man runs marathon after having a cardiac arrest on the toilet
A man from Stalybridge put in a marathon effort to conquer the TCS 2024 London Marathon while raising funds for the British Heart Foundation (BHF).
-
 Magpie's Nest leads the way in Tameside's journey to net zero
Magpie's Nest leads the way in Tameside's journey to net zero
A Stalybridge business has taken significant strides towards reducing its carbon footprint while promoting active travel and supporting local businesses.
-
 Award-winning Denton apprentice Billy is 'the embodiment of everything inclusion and disability service is about’
Award-winning Denton apprentice Billy is 'the embodiment of everything inclusion and disability service is about’
An apprentice with Active Tameside’s Everybody Can adult day service has been recognised by his training provider – the latest chapter in a journey that has seen him go from service user to provider.
-
 The Herbert Protocol continues to help save lives as GMP adopt online portal
The Herbert Protocol continues to help save lives as GMP adopt online portal
GMP have now adopted the online portal and form for the Herbert Protocol.
-
 United fan banned for three years after gesturing towards Liverpool fans
United fan banned for three years after gesturing towards Liverpool fans
A football fan has received a ban for mocking Liverpool fans at Old Trafford
-
 Ashton's Royal Mail delivery office to remain permanently closed
Ashton's Royal Mail delivery office to remain permanently closed
Ashton's Royal Mail Delivery Office will be remaining permanently closed, following previous plans for a temporary relocation.
-
 Tameside’s women in business celebrated in successful event by Bromleys Solicitors
Tameside’s women in business celebrated in successful event by Bromleys Solicitors
Tameside Women in Business (TWIBs) made a triumphant return this week with their first event of 2024, celebrating women in enterprise from Tameside and beyond.
-
 Tameside volunteers sign up as ‘Stage Guardians’ for the GM Ringway
Tameside volunteers sign up as ‘Stage Guardians’ for the GM Ringway
Three volunteers from Tameside have been recruited as ‘Stage Guardians’ for the GM Ringway, Greater Manchester’s walking trail.
-
 More than half of people with food allergies have had a reaction from mislabelled or unclear food packaging, new data finds
More than half of people with food allergies have had a reaction from mislabelled or unclear food packaging, new data finds
More than half of people with food allergies (56 per cent) have had an allergic reaction from mislabelled or unclear food packaging, with 23 per cent having suffered multiple reactions.
-
 Tameside Scouts mark St George's Day
Tameside Scouts mark St George's Day
More than 100 Scouts, from nine Scout groups, took part in Sunday's St George's Day parade through Ashton, alongside Ashton Brass Band.
-
 Mayor plants Ashton tree to be a living symbol of peace
Mayor plants Ashton tree to be a living symbol of peace
On Wednesday, April 17, the Civic Mayor Tafheen Sharif planted a Peace Tree in the Memorial Gardens in Ashton-under-Lyne, on behalf of and in the presence of school children from six local schools.
-
 No smoking or drinking: 100-year-old Joan's secret to a long life
No smoking or drinking: 100-year-old Joan's secret to a long life
A centenarian at HC-One’s Stamford Court care home in Stalybridge celebrated her 100th birthday in style this April, and shared her secret to a long life.
-
 By George! A good time was had by all
By George! A good time was had by all
Waterloo and Taunton Conservative Club, Ashton-under-Lyne, celebrated St Georges Day, England's patron saint, with entertainment from James Llwellyn Burke.
-
 PHOTOS: The abandoned Hyde farm set to be redeveloped
PHOTOS: The abandoned Hyde farm set to be redeveloped
A Hyde farm, which was previously earmarked for Tameside's first solar farm, could soon house six new properties, if plans are approved.
-
 A farm that has become victim to fly-tipping touted for redevelopment
A farm that has become victim to fly-tipping touted for redevelopment
Dunkirk Farm in Hyde could soon be transformed into six new homes, if Tameside Council approves the plans.
-
 Stalybridge Spring Show: Full schedule for 2024 event
Stalybridge Spring Show: Full schedule for 2024 event
Members of the Stalybridge Festival Committee are in full swing, adding the final touches to their plans for the yearly Stalybridge Spring Show in Cheetham Park on Sunday, May 3.
-
 Ashton restaurant threatens to expose dine and dashers after they scarper leaving £159 bill for food and cocktails
Ashton restaurant threatens to expose dine and dashers after they scarper leaving £159 bill for food and cocktails
An Ashton restaurant has appealed for two suspected dine and dashers to do the decent thing and return to pay their bill.
-
 Sound of music at The Vale as venue announces new gigs
Sound of music at The Vale as venue announces new gigs
The Vale has announced its new season, with three gigs specially selected to put a spring in your step.
-
 Mooch and natter in Mossley this May with the 2024 GM Walking Festival
Mooch and natter in Mossley this May with the 2024 GM Walking Festival
Explore Micklehurst and Midge Hill with a free photography walk this May as Mossley celebrates National Walking Month and the GM Walking Festival.
-
 Hyde theatre receives £20K funding boost from the People's Postcode Lottery
Hyde theatre receives £20K funding boost from the People's Postcode Lottery
Hyde Festival Theatre has been awarded a significant grant of £20,000 from the People’s Postcode Lottery.
-
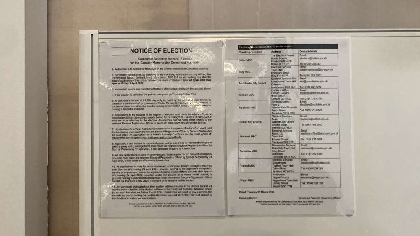
 TAMESIDE: What each political party in Tameside is offering to voters at the local elections this year
TAMESIDE: What each political party in Tameside is offering to voters at the local elections this year
Voters across Tameside will head to the polls to decide who their new councillors will be for the next four years come May 2.
-
 We asked every Greater Manchester mayoral candidate the same questions – this is what they said
We asked every Greater Manchester mayoral candidate the same questions – this is what they said
Greater Manchester residents will head to the polls in a fortnight — to not only decide who should run their councils, but also to select a mayor.
-
 "The pandemic changed my outlook on life": The Denton mum who started a business from her bathroom
"The pandemic changed my outlook on life": The Denton mum who started a business from her bathroom
Megan Montgomery found a new lease for life after starting Happy Houndz (Doggy Daycare & Dog Groomers) with her partner Nick Murray.
-
 The four Tameside planning proposals approved today, including an Aldi and Costa
The four Tameside planning proposals approved today, including an Aldi and Costa
A new Aldi and drive-thru Costa will be built just off Hattersley town centre now plans have been given the green light.
-
 Ashton woman takes on London Marathon to raise vital funds for women with ovarian cancer
Ashton woman takes on London Marathon to raise vital funds for women with ovarian cancer
Daisy Dixon, from Ashton, is fundraising for Target Ovarian Cancer in memory of her childhood best friend Johannah.
-
 "You've got your babies in the car": Women brawl in Denton rush hour row
"You've got your babies in the car": Women brawl in Denton rush hour row
Two women were spotted brawling at 8:15am this morning, April 17, in Denton.
-
 "A dream come true": Ashton under-10s dance team crowned British Champions
"A dream come true": Ashton under-10s dance team crowned British Champions
After putting their best foot forward at the British Open Championships in Blackpool Winter Gardens, an Ashton-based team of under-10s have earned the title of British Champions.
-
 Candy's Cupcakes thinks green
Candy's Cupcakes thinks green
A Tameside resident who runs a cupcake business in the borough has actively made changes to "Think Green" and be more environmentally friendly.
-
 New football pitch and cricket nets to be built inside Mossley factory
New football pitch and cricket nets to be built inside Mossley factory
A new sports facility containing a football pitch and cricket nets will be built inside a glass manufacturing factory in Mossley.
-
 Dukinfield Care Home rated in top 20 in the North West for fourth year running
Dukinfield Care Home rated in top 20 in the North West for fourth year running
HC-One’s The Beeches in Dukinfield are celebrating success after residents and relatives voted them as one of the Top 20 recommended care homes in the North West in the Carehome.co.uk Awards 2024.
-
 Tameside mum takes on Manchester Marathon challenge to raise funds for cancer unit
Tameside mum takes on Manchester Marathon challenge to raise funds for cancer unit
A remarkable mum is celebrating this week after taking on the Manchester Marathon to raise money for Tameside Hospital’s Breast Unit, which she says saved her life following a cancer battle.
-
 Hattersley apartment block hits new heights with major construction milestone
Hattersley apartment block hits new heights with major construction milestone
The partnership delivering 91 new apartments for over-55s in Hattersley has celebrated a significant construction milestone, after the state-of-the-art building reached its highest point.
-
 Young people are cooking up a treat at Care Leavers Teatime Club
Young people are cooking up a treat at Care Leavers Teatime Club
A new weekly club is offering care leavers the chance to learn cooking skills and enjoy a hot meal together.
-
 Stalybridge Street Fest is back for another year
Stalybridge Street Fest is back for another year
Stalybridge Street Fest is back for another year with a whopping eight food and family fun events set to bring a menu of tasty treats from April to November for 2024.
-
 Stalybridge woman "embracing a whole new life" after she used to dread leaving the house
Stalybridge woman "embracing a whole new life" after she used to dread leaving the house
Just over a year ago Sarah Speight was 25 stone, dreaded leaving the house and hated the thought of exercise.
-
 Charity event celebrating "All Things Women" heads to Stalybridge this month
Charity event celebrating "All Things Women" heads to Stalybridge this month
Mark your calendars for "All Things Women" on Friday, April 26, at Industry in Stalybridge.
-
 Mother and daughter from Hyde banned from keeping animals after RSPCA prosecution
Mother and daughter from Hyde banned from keeping animals after RSPCA prosecution
A mother and daughter from Hyde have received bans on keeping animals following an RSPCA prosecution after neglected horses, lame goats and sick pets were found at an animal rescue centre.
-
 Woman's terrified 999 call after car thief kidnapped her 89-year-old mother
Woman's terrified 999 call after car thief kidnapped her 89-year-old mother
Police have released the terrified emergency ca.ll made by a daughter after a thief stole her car while her mother was sitting in the passenger seat
-
 Thief sentenced to eight years for kidnap after stealing car with woman, 89, in passenger seat
Thief sentenced to eight years for kidnap after stealing car with woman, 89, in passenger seat
A man has been jailed for stealing a car while an elderly woman was sitting in the passenger seat
-
 UPDATE: Fire fighters tackle huge moorland blaze
UPDATE: Fire fighters tackle huge moorland blaze
Fire fighters from Glossop were tonight battling a huge moorland fire.
-
 BREAKING NEWS: Huge fire spotted near Snake Pass
BREAKING NEWS: Huge fire spotted near Snake Pass
A huge bank of flames has been spotted by drivers on the Snake Pass.
-
 Everything due to go before the planning panel in Tameside next week
Everything due to go before the planning panel in Tameside next week
A new Aldi superstore and a Costa drive-thru are set to get the go-ahead in Hattersley, if the planning panel approve it.
-
 PEER-ing ahead to better support
PEER-ing ahead to better support
People with a learning disability in Tameside will soon benefit from improved support, thanks to the introduction of Greater Manchester’s first learning disability peer support workers.
-
 206 per cent surge in refugee minors in Tameside in just a year
206 per cent surge in refugee minors in Tameside in just a year
The latest available figures reveal a 206 per cent surge in the number of refugees, asylum seekers and immigration applicants under 18 residing in Tameside, within just a year.
-
 Bands strike up again for the Tameside Whit Friday Contests
Bands strike up again for the Tameside Whit Friday Contests
It's Whit Friday on May 24, and once again Tameside will be hosting the hugely popular brass band contests which are often billed as the greatest free show on earth.
-
 Tameside-based solicitors raise hundreds of pounds for local hospice
Tameside-based solicitors raise hundreds of pounds for local hospice
Through colleague fundraising efforts, Bromleys Solicitiors have raised £862.50 for their nominated Charity Partner, Willow Wood Hospice.
-
 Investigation launched after man dies in Droylsden house fire
Investigation launched after man dies in Droylsden house fire
Forensics and fire crews remain at the scene today after a man died in a house fire in Droyslden last night, Tuesday 9 April.
-
 Police appeal to find man wanted for making threats to kill
Police appeal to find man wanted for making threats to kill
Police have issued the mugshot of a man from Tameside wanted for making 'threats to kill'.
-
 Hyde man fined for dumping his rubbish in neighbouring street
Hyde man fined for dumping his rubbish in neighbouring street
A man has been fined by Tameside magistrates for flytipping his household waste in a neighbouring street.
-
 Dukinfield shop owner fined for sale and supply of illicit tobacco
Dukinfield shop owner fined for sale and supply of illicit tobacco
A Dukinfield shop owner has been ordered to pay more than £1000 by Tameside magistrates after pleading guilty to four charges in relation to the sale and supply of illicit tobacco.
-
 Man arrested and drugs recovered from toilet u-bend after morning warrants in Hyde
Man arrested and drugs recovered from toilet u-bend after morning warrants in Hyde
Class A drugs and other paraphernalia were recovered this morning as GMP's Challenger team provided an early morning wake-up call to those suspected of criminality in the Tameside area.
-
 Shop fined for underage e-cigarette sale
Shop fined for underage e-cigarette sale
A Shop has been ordered to pay £1300 for selling an e-cigarette to an underage person during a Tameside Trading Standards operation.
-
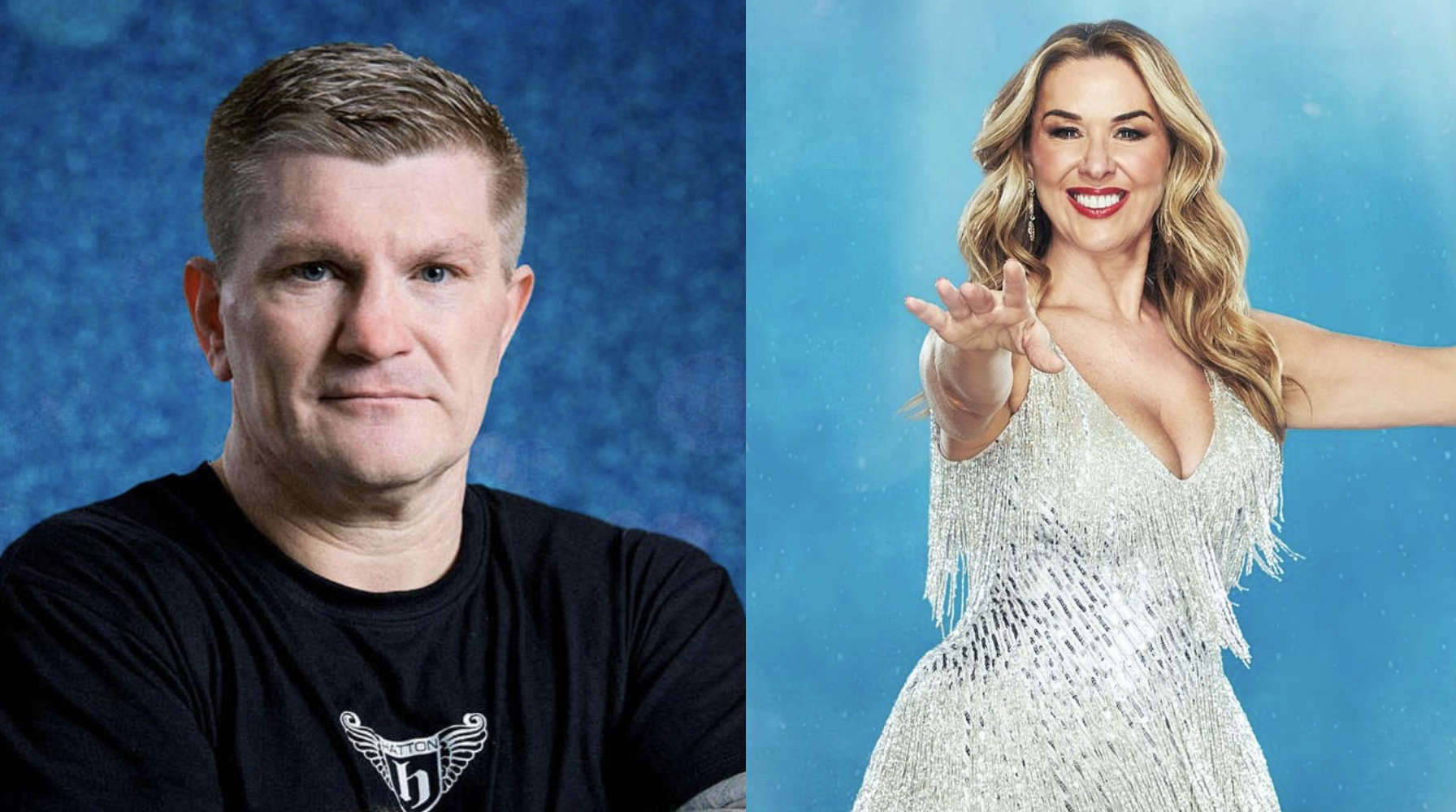 Ex-boxing champ Ricky Hatton steps out in Hyde with Dancing on Ice co-star Claire Sweeney
Ex-boxing champ Ricky Hatton steps out in Hyde with Dancing on Ice co-star Claire Sweeney
Ricky Hatton has reportedly been spotted "cosying up" to Dancing on Ice co-star, Claire Sweeney, on a night out in Hyde at the weekend.
-
 GHOST The Musical comes to Mossley this month
GHOST The Musical comes to Mossley this month
Join award-winning Mossley AODS (Amateur Operatic & Dramatic Society) as they bring the story of GHOST The Musical to The George Lawton Hall from Tuesday 23 to Saturday 27 April.
-
 Denton theatre group to put bullying under the spotlight with new production
Denton theatre group to put bullying under the spotlight with new production
A Denton-based theatre group recently welcomed two guests to observe rehearsals for their new show which delves into online safety and combating bullying on social media.
-
 TAMESIDE: All the candidates standing in the 2024 local elections in Tameside
TAMESIDE: All the candidates standing in the 2024 local elections in Tameside
The local elections next month are looming, and dozens of hopeful candidates will be vying for one of the 19 seats on the council.
-
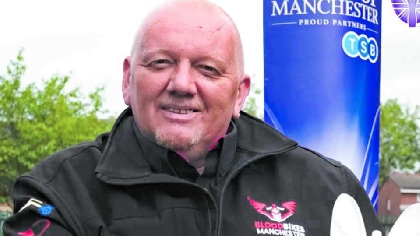 Bikers pay funeral tribute to founder of Blood Bikes Manchester charity
Bikers pay funeral tribute to founder of Blood Bikes Manchester charity
Bikers took to the streets in Tameside to pay tribute to Paul Redfern, founder of the Blood Bikes Manchester charity who died following a two year battle with lung cancer.
-
 Emmaus Mossley to host Secondhand Superstore Spring Sale
Emmaus Mossley to host Secondhand Superstore Spring Sale
Homelessness charity Emmaus Mossley is gearing up for a special Spring-themed charity event on Saturday 20 April at their large Secondhand Superstore.
-
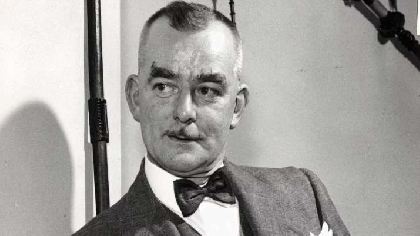 Drinkers didn't suspect landlord was Ashton raised last hangman Harry Allen
Drinkers didn't suspect landlord was Ashton raised last hangman Harry Allen
Apart from the regulars, few visitors to Harry Allen’s pub could imagine the macabre secret of the dapper bow-tied man pulling them a pint.
-
 Hundreds of Tameside residents receive accredited training qualifications
Hundreds of Tameside residents receive accredited training qualifications
More than 220 people across Tameside have upskilled and received valuable learning qualifications through a range of training courses offered by a local housing provider.
-
 GREATER MANCHESTER: All the key developments submitted across Greater Manchester this week
GREATER MANCHESTER: All the key developments submitted across Greater Manchester this week
A huge hotel expansion and the conversion of a historic building into new homes are the highlights of this week’s planning applications.
-
 GREATER MANCHESTER: Full list of Mayoral candidates confirmed
GREATER MANCHESTER: Full list of Mayoral candidates confirmed
The list of candidates for this year’s Greater Manchester mayoral election has been confirmed.
-
 Local football fans raise almost £4K for Willow Wood Hospice
Local football fans raise almost £4K for Willow Wood Hospice
Eleven local lads have raised just under £4,000 for Willow Wood Hospice through a charity walk they took part in on March 23.
-
 Andy Burnham launches mayoral re-election campaign with a favourite fab four tune
Andy Burnham launches mayoral re-election campaign with a favourite fab four tune
For a politician who’s had to convince Greater Manchester he’s not a Liverpudlian lad, it was an odd choice to play ‘Penny Lane’ by The Beatles at Andy Burnham’s campaign launch.
-
 Eight charities successfully bid for funding in Dragons' Den competition
Eight charities successfully bid for funding in Dragons' Den competition
Charities were successful in their pitches for funding from Dukinfield and Stalybridge Rotary Club’s annual Dragons' Den.
-
 Bus company donates Easter gifts to local hospital
Bus company donates Easter gifts to local hospital
Stagecoach Manchester has donated around 200 Easter gifts to children at the Tameside and Glossop Integrated Care NHS Foundation Trust.
-
 Two Tameside residents among new Deputy Lieutenants commissioned in Greater Manchester
Two Tameside residents among new Deputy Lieutenants commissioned in Greater Manchester
The Lord-Lieutenant of Greater Manchester, Diane Hawkins JP LLB, has appointed new Deputy Lieutenants, two of whom are Tameside residents.
-
 Andy Burnham apologises after week of bus disruptions
Andy Burnham apologises after week of bus disruptions
Commuters were left stranded across Oldham this week after delays and cancellations blighted the borough’s brand-new bus system.
-
 Guide dog trainee Ralph sponsored by Tameside businessman
Guide dog trainee Ralph sponsored by Tameside businessman
Puppy Ralph chomps on a bone as he takes a break from his training to be a guide dog.
-
 Police in Tameside band together to buy a bed for a child in need
Police in Tameside band together to buy a bed for a child in need
Officers and staff from GMP Tameside Prevention Hub have been working closely with young children to keep them out of crime and break the viscous cycle of gang recruitment by safeguarding those at risk of being lured into organised crime.
-
 Ashton pub devastated by burglary in early hours
Ashton pub devastated by burglary in early hours
A pub in Ashton has been left devastated after a burglary at 3am this morning, April 4.
-
 GM Ringway and Forever Manchester team up for a major summer fundraiser
GM Ringway and Forever Manchester team up for a major summer fundraiser
The GM Ringway, Greater Manchester’s walking trail, has teamed up with the charity Forever Manchester to raise vital funds for community projects across the city-region.
-
 Four in ten people in the North West are 'economically inactive', says report
Four in ten people in the North West are 'economically inactive', says report
New findings reveal that human health and social work is the most common industry for North West residents to work in.
-
 Andy promises hopper fares on Greater Manchester's buses if re-elected as mayor
Andy promises hopper fares on Greater Manchester's buses if re-elected as mayor
Hopper fares will be introduced on Greater Manchester’s buses if Andy Burnham is re-elected, the mayor has promised.
-
 “They just don’t listen” - Denton resident rooted in battle with council over pavement problem
“They just don’t listen” - Denton resident rooted in battle with council over pavement problem
Ged Redman of Windsor Road Denton has spoken out against the council amidst new works going on in front of his house, which has caused further damage to a large tree.